| Messing
with Mother Nature
By Lindsay Heintz
OTTAWA — For
Lori Tarbett, Depo-Provera seemed like a wonder drug.
The 21-year-old was in a committed
relationship and looking for a low-maintenance birth
control method. Like other young women, she was attracted
to the idea of a birth control injection every three
months and the sexual freedom the drug promised. She
also liked the idea of not getting her period, a symptom
of the injection that most women experience, which could
alleviate painful side effects of menstruation.
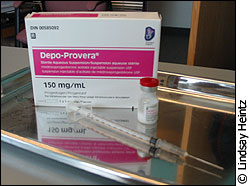 |
| Depo-Provera, an injectable
for of birth control. |
“I started taking it because
I was having problems with the Pill — having chest
pains,” she said. “I’d always had
really bad [period] cramps, to the point that I would
have to leave school sometimes.”
Almost immediately, the drug started
to lose its appeal. Beside weight gain, major mood swings
and decreased sexual libido, Tarbett suffered from continuous
bleeding when she expected her periods to stop. After
three injections, she called it quits.
“I took it because I wanted
to make my relationship better; I could have sex whenever
I wanted, and I thought, ‘that’s great —
a shot every three months,’” she said. “But
I didn’t even want to have sex, and when you’re
bleeding all the time it’s not the most attractive
thing.”
Eliminating the inconvenience
Drugs like Depo-Provera, an injection
of progesterone given every three months, and Seasonale,
an oral contraceptive designed so women only menstruate
four times per year, are the primary methods of suppressing
menses. Some women are advised by their physicians to
take their 28-day cycle oral contraceptives continually,
without taking a break each month for their period.
Dr. Christine Hitchcock, a research
associate at the University of British Columbia, said
she feels convenience is the main reason women choose
to suppress their periods.
“People isolate menstruation
from the female body - they think it only has to do
with fertility, and if you’re not trying to get
pregnant what’s the big deal?” said Hitchcock.
“Hormones are a whole part of our health as women;
it’s a lot more than bleeding and babies.”
Dr. David Pfeiffer, director of Health
and Counselling Services at Carleton University, says
there are circumstances when women should look at menstruation
suppression as an alternative to getting their period
every month.
| 'You have
to wonder if it’s a good idea to be adding
pharmaceuticals to our bodies for convenience rather
than necessity.' |
“Certainly if you’re travelling
somewhere where it’s not convenient, it‘s
not really a problem,” said Pfeiffer. “But
if you’re a woman who’s having major problems
with your period, it’s something that should be
looked at.”
Pfeiffer said some conditions are triggered
by menstruation, including menstrual migraines, certain
forms of epilepsy and endometriosis — where tissue
formed along the uterus lining binds to other organs,
causing extreme pain. For women suffering from these
ailments, Pfeiffer said not having a period could be
an alternative.
“I don’t think there’s
any evidence that it’s harmful to a woman,”
said Pfeiffer. “But it’s kind of fiddling
with things — and you have to wonder if it’s
a good idea to be adding pharmaceuticals to our bodies
for convenience rather than necessity.”
The medical evidence
Research shows there may be dangerous
side effects of menstruation suppression drugs. Besides
decreased libido, weight gain, and breakthrough bleeding
cautioned by drug manufacturers of Depo-Provera and
various oral contraceptives, there is also evidence
of an increased risk for osteoporosis.
 |
| Ortho Tri-Cyclen, a birth
control pill. |
A study published in the British Medical
Journal found that women aged 18 to 33 taking Depo-Provera,
oral contraceptives or non-hormonal birth control, those
on Depo-Provera for two years experienced an average
bone density loss of 5.7 per cent. Similarly, a study
in the Canadian Medical Association Journal
found that women who were taking oral contraceptives
had an overall lower spinal and neck bone density than
those on non-hormonal forms of birth control. The CMAJ
report concluded that the lower bone density values
in oral contraception users could translate to an increase
in fracture risks of 20 to 30 per cent, in relative
terms.
Dr. Hasnain Khandwala, an endocrinologist
at the University of Saskatchewan, said suppressing
menstruation causes a decrease or elimination in the
production of estrogen. Drugs like Depo-Provera suppress
the production of ovarian estrogen. He said bone formation,
reaching a peak in production when women are in their
late 20s and early 30s, is dependent on estrogen, which
stimulates bone cells. Khandwala said while it may be
possible for women who suppress menstruation to regain
their bone density, it is not guaranteed.
There may also be a possible link between
suppressing menstruation and an increased risk for heart
disease. According to the medical journal Heart,
women have a lower incidence and death rate from coronary
heart disease than men — and the medical community
has never been able to explain the difference. While
it has been theorized that female estrogen production
protects women from heart disease, a controversial iron
hypothesis explains the difference another way.
Dr. Jerome Sullivan developed the hypothesis
which suggests that iron lost through menstruation protects
women from heart disease. Sullivan proposes that increased
iron in the blood increases the levels of low-density-lipoprotein
(LDL) cholesterol, which can increase one’s risk
for heart disease. Sullivan also points out that menopausal
women accumulate iron levels in their blood roughly
equal to men; therefore he theorizes that menstruating
women are protected by their periods.
Hitchcock said while there may be risks
associated with an absence of menstruation, she is more
concerned with a lack of data proving the practice is
safe.
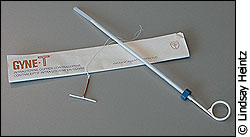 |
| Intra Uterine Device |
“When you’re looking at the
studies and data on this, it’s amazing what people
aren’t looking for,” she said. “It’s
quite possible there are no risks associated with not
having a period, but I don’t think we have enough
data to say if this is a good practice.”
A woman's choice?
Doctors like Dr. Roger Pierson, a professor
of obstetrics and gynecology at the University of Saskatchewan,
feel the choice of contraception is a decision best
left to women.
“I’ve never had a period,
nor do I plan on getting one, so we as doctors need
to provide women the information so they can make the
best choice for themselves,” said Pierson. “However
the notion that we need to have a period every month
is more of a sociological, rather than biological belief
- if you’re not trying to get pregnant, you don’t
really need to get it.”
Dr. Ingrid Johnston-Robledo, a professor
of psychology at the State University of New York at
Fredonia, said the practice is part of a trend to treat
menstruation as a medical problem.
“We’re viewing menstruation
as if it needs to be cured, and we’re appealing
to women by focusing on all the negative aspects of
having a period,” she said. “Women’s
reproduction is being pathologized, and made to seem
like menstruation is a burden with work, academics,
our social life.”
 |
| Condoms, a non-hormonal birth
control. |
Hitchcock said women aren’t being
informed about the risks of suppressing menstruation.
Until the medical community can prove there aren’t
major health risks, she said it shouldn’t be promoted
to women.
“We have a history of medical
interventions in women’s health that have been
applauded and lauded, and have turned out to be disastrous,”
she said. “Medicine has gotten it wrong in significant
ways.”
|