|
| A mysterious parasite
At first, he thought it was the flu – with its symptoms of a fever, chills, vomiting and fatigue. But after his skin started tingling and he started convulsing, Whitaker concluded it wasn’t. He was right. It was malaria – a disease with symptoms that are similar to the flu. The diagnosis was a shock to the 25-year-old student from Sidney, B.C. True, he had spent his summer volunteering in Burkina Faso – a small west African nation – but he had been home now for over five weeks. “It felt like nothing I had ever experienced,” said Whitaker. “I knew something was horribly wrong. But I couldn’t put my finger on what it was.”
Whitaker’s doctors were also baffled. As Whitaker returned again and again to the hospital, with increasingly severe symptoms, his doctor stabbed and prodded him, trying to find out what the problem was. Over a week later, they came to the conclusion that although he had been taking anti-malarial drugs while in Burkina Faso, Whitaker was still at risk for malaria. To diagnose malaria, a blood test is done which detects malarial antigens and the density of them on the blood smear. In Whitaker’s case, his test came back positive. “My doctors had no idea what was going on,” says Whitaker. “It was like the blind leading the blind.” The challenge of fighting malaria Malaria is a parasitic disease that infects over half a billion people every year and kills more than a million people. It’s both preventable and treatable. The parasite is picked up from the blood of an infected person and passed on to a healthy human being by the female Anopheles mosquito. Despite scientific advances, the number of cases of malaria is increasing every year.
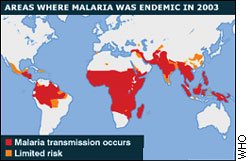
The disease is most commonly found in tropical places – particularly Sub-Saharan Africa. But the disease also exists on Canadian soil – when Canadians travel abroad, return home, and later develop the disease. But problems arise when Canadian doctors, who can’t fathom the idea of a Canadian patient contracting malaria, don’t diagnose the disease quickly Creating a "dipstick on steroids" Dr. Kevin Kain, a malarial researcher at the University of Toronto, is trying to come up with a way to make sure people like Whitaker know right away that they have the malaria parasite and how to treat it.
Kain is currently developing a “blackberry for infectious diseases,” a small, hand-held diagnostic device which use a small blood test to diagnose malaria in 20 minutes. “What we really want to do is build a dipstick on steroids,” he says. “Something that can detect multiple infections simultaneously, produce automated feedback to the user to say, ‘this is the pathogen, this is therapy you should use and this is the public health or infection control issues that are associated with this pathogen.” The commonly used diagnostic tool for malaria now is a microscope which examines a blood smear. Kain says this is slow, antiquated, and most importantly – often wrong.
At the moment, Kain’s device is the size of a small table and Kain says this needs to shrink drastically in size. It’s also too expensive – for either hospitals in North America or other malaria-affected areas like Africa. “It’s still being developed,” says Kain. “But we can build technologies that can provide so much medical information to a user that I think it will have a major technologic breakthrough,” he says. The affordability factor Timothy Stone is another Canadian researcher who studies infectious diseases in tropical areas. He says that something like the dipstick test is still years away “My concern is that it will never be affordable for those who need it most,” he says. “For the people in Sub-Saharan Africa.”
Kain counters that even five years ago, the number of cell phones in Africa was miniscule. Now, their numbers have boomed, far outnumbering the number of land-line phones in the country. He says it’s just going to be a matter of time (three to five years, he estimates) and that it’s entirely possible to see his “dipstick test” in a similar way. Kain says he has been interested in malaria since he took a trip to Africa decades ago. He says that the number of people dying from malaria is barely a blip on the North American spectrum – simply because malaria is seen as something that is happening far away. He adds that every 30 seconds a child dies of malaria. “If that kind of a thing was happening in Europe or North America, there’d be outrage, there would be demands for action,” he says. “It’s an appalling statistic and an appalling response.” The Canadian connection Kain says that regardless of what most people might think, being a malarial researcher based in Canada is valuable. “Canadians are like canaries in coal mines,” he says, adding that Canadians travel all around the world, get malaria, and come home. This helps Kain’s research by providing a wide geographical survey of different types and strengths of malaria and a wide variety of people to do testing on. Four hundred to 1,000 Canadians are infected with malaria annually, four to 10 times the per capita rate reported in the U.S. It’s thought that these rates may be under-reported – often because doctors misdiagnose malaria in Canadian patients.
Kain says his dipstick test could change the fate of many African children, in addition to diagnosing Canadian patients sooner, and more accurately. “This could change the way we diagnose malaria,” he says. “For the better.” But even for someone like Whitaker, even if he finds out he has malaria, he could be plagued with the disease for years to come. Malaria has a nasty habit of recurrence - some patients have been infected 35-40 times again in several years after the first attack. There is nothing people can do to prevent this. Life after malaria Whitaker says he wishes something like Kain’s dipstick test existed when he was suffering from malaria. He says, although he didn’t die, he could have, and that a test like this would have been able to diagnose his disease far more quickly. “I was off work for 8 weeks,” he says. “It was terrible. Sometimes I think to myself, ‘What if they had caught it earlier? Would it have been easier? Would my recovery time have been shorter?” “Who knows,” he adds. “But I sure wish malaria had been on the radar of the doctors at the hospital.” Whitaker goes on to say that he welcomes the technological idea of having a portable dipstick test, even if it takes years to develop. “What an interesting idea,” says Whitaker. “This device could have an amazing impact on not just Canadian suffering from malaria, but for people around the world.” “It could have changed my life.”
|
|
|