|
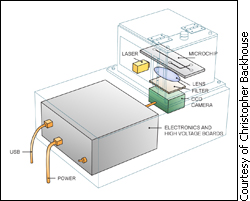
The goal is to replace conventional lab equipment with an integrated and automated genetic-testing unit that can bring results to the patient quickly, said Christopher Backhouse, a professor at the electrical and computer engineering department. “It’s our mission to drop the ultimate cost by a factor of a million,” he said. Backlogged labs and high prices often hinder the tests, which can help spy elusive viruses; diagnose cancer; and pinpoint the correct drug dosages for patients. Backhouse, with colleague Linda Pilarski, an oncology professor, and their research team have succeeded in building a shoebox sized, portable unit that costs only $1,000. In January 2008, the Analyst, a journal put out by the U.K. based Royal Society of Chemistry, published an article where journal staff touted the unit as a critical advance for the so-called “lab-on-a-chip” technology. They wrote, “Canadian scientists have succeeded in building the least expensive portable device for rapid genetic testing ever made.” The core of the unit is the microchip made of polymer and glass, which is about the size of a standard microscope slide. Etched onto two glass layers are tiny channels – barely a hair’s breadth wide – separated by a thin titanium membrane that traces the route to reaction chambers where the tests are performed. “The chip replaces almost a quarter of the equipment in my research lab,” said University of Alberta’s Pilarski. She said the research team is working to fully automate the unit so the lab technician need only load the sample, push the on button and wait for the read out. But the chips aren’t discovery tools to determine what genes cause what disease – they can only be programmed to test for known patterns, she said. Backhouse said he hopes doctors will eventually use the unit to help reduce the number of people who die each year of adverse drug reactions. “When we’re diagnosed, physicians tend to assume we’re all the same,” he said. “But treatment that might help one person could be toxic to another.” Taking the stress out of the test The chips could also screen for diseases and cancers that are either too complex or too expensive to do at a regular walk-in-clinic. And having genetic testing readily available could help detect what conventional tests might miss. Barrie, Ont, resident Roger Madill, 65, knows how important this can be. At his annual checkup in 2000, his doctor recommended the prostate specific antigen (PSA) exam, which is regarded as one of the best early-detection tests. Though the results indicated his PSA levels were low – and consequently fit the norm for his age group – Madill opted to get “the rubber glove” anyways. A week later he was diagnosed with prostate cancer and three months later he was laying in a hospital bed prepping for surgery.
His journey didn’t stop there though, the cancer came back and Madill had to undergo radiation therapy. Now, every six months, he goes to the hospital to make sure the cancer hasn’t returned. “You can brainwash yourself into thinking ‘what will be will be,’” he said. “But it doesn’t do anything until you hear the word ‘negative.’” He said he doesn’t let the fear of a relapse rule his day-to-day life, but usually in the two weeks leading up to the test unease settles in the pit of his stomach. “I’m starting to get used to it,” he said. “But it’s hard not to think about it coming back, especially since I’ve already had a reoccurrence.” The stress of waiting for results is one factor the lab-on-a-chip technology could help reduce, said Pilarski. The Future Backhouse said that the team is continuing to adapt and reconfigure the existing technology to simplify its use. He compares it to the evolution of computers.
“You used to need a PhD to operate one, now they’re in kindergarten classes,” he said. The research team has spent 10 years developing the technology that led to the shoebox sized unit. In five years, Backhouse said he hopes to reduce its size to that of a USB key, with the cost hovering somewhere around $10. But the technology will have to undergo rigorous testing and review before it can be applied in doctors offices or be sold over the counter. Pilarski said there are concerns with providing tests to people without medical consultation. She said though a test might give a percentage giving the likelyhood of contracting a disease, people might panic because they don't understand the statistic. "It could make people think they're sicker than they really are," she said. Backhouse adds society should start considering how to regulate genetic testing in the field before it becomes too mainstream. “We need to start setting the precedent,” he said of the emerging technology. “It won’t be long before these chips and other like them will be sold over the counter at the corner store.”
|
|
|